Cold winter temperatures can cause an increased risk of health problems and weather-related injuries for older adults. Hypothermia, frost-bite, influenza and falls in the ice or snow can present major health concerns during the winter months. Because older adults lose body heat faster than compared to their younger years, staying warm enough during the winter can be a challenge. In fact, according to the Centers for Disease Control and Prevention, adults ages 65 and older are at a high risk of developing complications, such as pneumonia from the flu. Flu activity is the highest between December and February, and can last until the springtime. While the flu might seem like a nuisance for many people, it can cause serious health complications for older adults, especially for those with weakened immune systems.
Complications from Influenza
Influenza in older adults triples the risk of both heart attack and stroke within the first two weeks of infection. Pneumonia, which is an infection of the air sacs in one or both of the lungs, is characterized by severe cough, fever, chills and difficulty in breathing. Pneumonia often occurs as a complication of influenza and can cause serious health problems, including death, for older adults. If you have been ill with influenza and experience severe coughing with large amounts of mucus, trouble breathing, shortness of breath, severe chills or sweating, a fever higher than 102 degrees Fahrenheit, and chest pains, contact your healthcare provider immediately.
Tips for Preventing Winter Illness
Get the flu and pneumonia vaccine
The Centers for Disease Control and Prevention advise older adults to get the flu vaccine each year starting in September. The vaccine is proven to be the best way to protect against influenza and its complications. Flu vaccines are updated each season and can reduce the severity and duration of the illness. Older adults should also consider getting the pneumonia vaccine, as the illness can cause severe problems.
Practice good hygiene
Germs from your hands can enter through your nose and mouth, causing you to become ill. Make sure to wash your hands with soap and warm water to disinfect any germs and prevent illnesses from entering your body. Use antibacterial hand sanitizer when on the go.
Wear a mask
Wearing a mask isn’t only preventative towards COVID-19. In fact, wearing a mask when in public can help prevent the spread of the flu and other wintertime illnesses. It’s also important to wear a mask when you are ill or feel an illness coming on to protect others from getting sick.
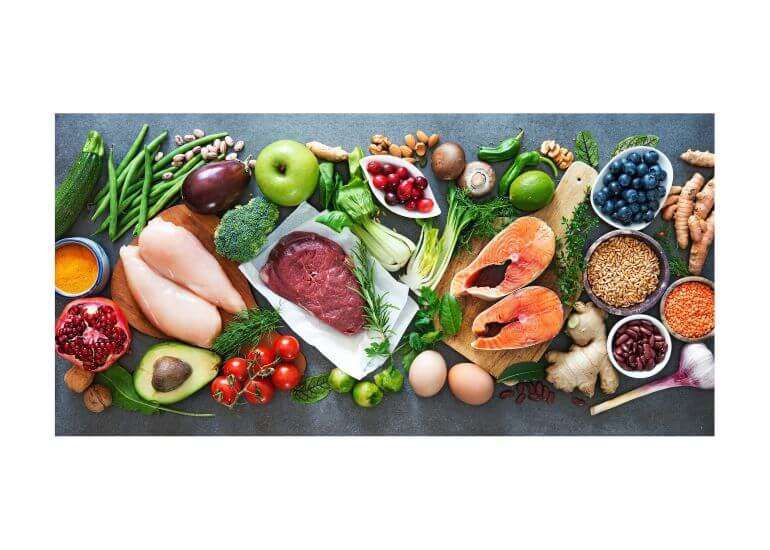
Eat a healthy diet
Eating a well-balanced diet of fruit and vegetables can help keep the immune system functioning and even reduce the risk of developing wintertime illnesses such as influenza and the common cold. Staying hydrated also helps the body fight off infections. Studies have shown that foods high in vitamin C such as citrus fruits, peppers and broccoli can help boost the immune system and prevent illness.
Avoid touching your face
You may touch your face more often than you think! However, during the flu season it’s important to keep your hands away from your nose and mouth, as germs can enter the body and cause us to get sick.
Clean high touch surfaces
It’s important to consistently disinfect common areas in your home such as the kitchen and bathroom. Germs can multiply even in your home and increase the risk of developing influenza and other illnesses. Keep disinfecting wipes easily accessible in high touch areas and use them on doorknobs, light switches and counters.
Staying Healthy at Maple Knoll Village
We know how dangerous the flu can be for our residents at Maple Knoll. That’s why our community provides the flu vaccine and healthy meal options which support an effective and strong immune system. How are you staying healthy this winter?